Mini IVF – Cost, Success Rates, Mini vs IVF Protocol Comparison
Mini IVF is in vitro fertilization with a reduced protocol. We also call it ‘gentle’, ‘mild’, ‘micro’, or low-stimulation IVF because it involves using small doses of medications to grow and retrieve eggs. Consequently, it decreases hormonal side effects and minimizes the risk of hyperstimulation.
Unlike the conventional program, mild IVF is primarily based on an oral medication instead of hormonal injections. This way, the patient receives fewer eggs than in the traditional method, however, it does not affect their quality. Mini IVF has a gentle effect and is optimal when the standard protocol can be harmful or irrelevant. Today, we are going to look at cases when it is better to choose slight stimulation, overview the prices, and share success rates of both IVF protocol types.

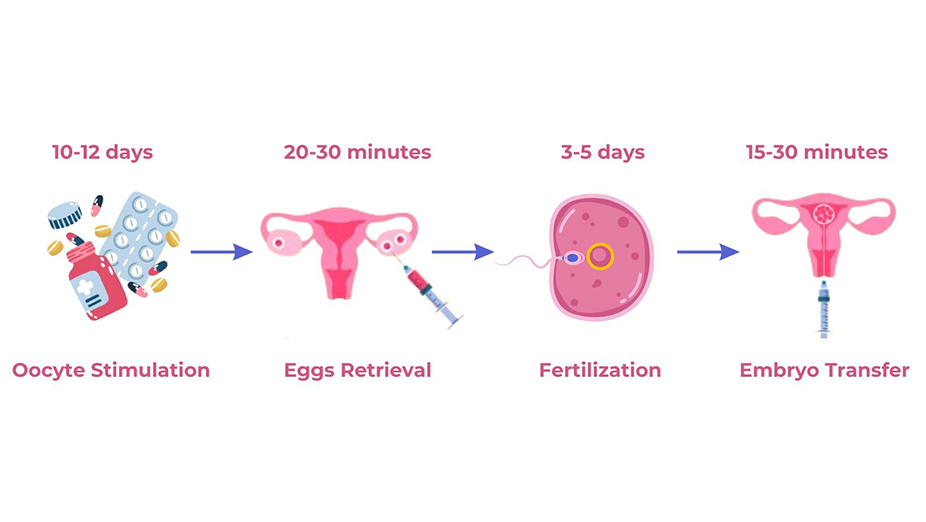
Mini IVF Protocol
The low IVF protocol is practically no different from the standard program. It is not simpler or faster than conventional IVF, but only milder in terms of drug selection. Let’s find out how it works in stages.
Mini IVF Ovarian Stimulation
Duration: 10-12 days.
Start: days 2-4 of the menstrual cycle.
Process: Before starting the first phase of micro IVF, our reproductive specialist measures hormone levels and follicular baseline. These indicators allow doctors to choose a complex of drugs for a successful pregnancy. We take tests every 2-3 days to monitor the uterine lining and follicular growth.
The most commonly used are preoral drugs, in particular, Letrozole. If an additional source of stimulation is needed, the doctor may prescribe injections with Follistim or Menopur. The therapy lasts about 10 days.
When the follicle size increases to 17-19 mm in diameter, the healthcare specialist changes the drug to help the eggs mature for further retrieval.
Eggs Retrieval
Duration: approximately 20-30 minutes.
Start: day 13 from the beginning of the IVF treatment.
Process: Our reproductive doctor retrieves follicles after the egg maturation. It is an outpatient procedure that is performed approximately 35 hours after taking the hCG hormone – the trigger that causes ovulation.
The procedure is performed transvaginally under general anesthesia or sedation. The eggs are collected using a puncture needle under ultrasound guidance. Material is carried to an embryologist to prepare for fertilization or freezing. It is possible to obtain 3-6 high-quality oocytes.
You may experience drowsiness, moderate pain in the lower abdomen, and scanty bloody vaginal discharge after egg retrieval. Recovery usually lasts 3-4 days.
Fertilization and Embryo Development
Duration: 3-5 days.
Start: 6-8 hours after egg retrieval.
Process: Fertilization occurs in two ways:
- We place the oocyte and sperm in a petri dish for natural fertilization when the sperm move to and penetrate the egg.
- A spermatozoon is injected into the oocyte using a hollow needle. It is called ICSI fertilization.
The embryos grow in an environment that mimics the fallopian tube. Usually, development takes 3-5 days. The grown blastocyst can be sent for genetic testing to exclude the risk of mutations or to select the sex of the future child.
Embryo Transfer
Duration: 15-30 minutes.
Start: days 17-20 of the woman’s cycle.
Process: The embryo transfer usually occurs on the 5th day of its growth, when it is at the blastocyte stage. The number of embryos is agreed with the doctor. It depends on the patient’s age and hormonal parameters.
So, the agreed number of cells is in an elastic catheter. It is inserted into the uterine cavity through the cervix. We perform these manipulations under the control of ultrasound. After the transfer, the embryologist checks the catheter under a microscope to ensure all the tissues have been transferred. It is painless, so it does not require anesthesia.
You may cryopreserve the leftovers for future cycles.
Micro IVF Medications
The main difference between mini IVF and other programs is a gentle treatment regimen. Our specialists choose milder drugs, rather than medicines in conventional IVF, that cause minimal harm to the body and, at the same time, have a positive effect. A well-selected complex leads to conception on the first try.
Below, you can see the medications most often used at each stage.
| Stage of IVF | Medications | Dosages/Instructions | Purpose |
|---|---|---|---|
| Stimulation | Letrozole | Typically 2.5-5 mg per day for 5-10 days | Inhibits estrogen production |
| Stimulation | Follitropin | Usually 75-150 IU daily | Encourage follicle growth and egg development |
| Stimulation | hCG in Profasi, Rotten, Lupron | Trigger shot; timing varies, usually when follicles are mature | Induces ovulation and prepares eggs for retrieval |
| Embryo Transfer and Post Transfer | Progesterone | The daily dose is up to 600 mg, taken within 12-14 weeks after the transfer | Prepares the uterine lining for implantation |
| Embryo Transfer and Post Transfer | Estradiol | 600-800 mg per day | Supports uterine lining thickening and receptivity |
| Embryo Transfer and Post Transfer | Duphaston | 30-60 mg per day, orally | Maintains the uterine environment for implantation |
Remember that this program is approximate and generalized. We strongly recommend consulting with a reproductive specialist to select an individual plan with drugs and dosages.
Low Stimulation Benefits
Reducing the number and doses of drugs has many positive consequences. First of all, it mitigates the risk of developing hormonal diseases. Also, this method decreases the cost of the procedure, which is relevant for many patients.
In a nutshell, the main reasons why customers prefer low therapy include the following:
- Reduce the likelihood of complications such as ovarian hyperstimulation syndrome. This pathology causes nausea, abdominal distension, and deterioration of a woman’s general well-being. It is a stumbling block to successful conception.
- Minimize the risk of a frozen pregnancy, which often occurs due to changes in the endometrium caused by excessive stimulation.
- Decrease the number of embryos. It is a significant advantage for ethical reasons. After the standard protocol, a certain number of embryos remain. They may be frozen or destroyed. When the worldview or the budget do not allow patients to accept either, the solution will be slight stimulation, during which the couple receives only 2-3 embryos.
Moreover, in case of an unsuccessful attempt, you may repeat treatment in the next cycle because the body does not need a long time to recover.
Mini IVF VS IVF – What Is The Difference?
Mild IVF differs from conventional IVF at the egg stimulation stage. It involves the use of less medication to grow follicles and induce ovulation. Moreover, this method concentrates on oral drugs and minimizes (if possible eliminates) injections. Once ovulation has begun, the rest of the procedure is very similar to standard protocol.
This video provides a comparison of the two programs and answers many burning questions, such as prices and results of the method.
What is Mini Stim IVF? Is Minimal Stimulation IVF Protocol Better Than Conventional IVF?
Who Should Consider Micro IVF?
Gentle fertilization shows high results and gives a chance for a pregnancy. It is relevant in the following cases:
- women under 40;
- patients with hormone intolerance;
- women with tubal ligation;
- LGBTQ couples;
- individuals with a small reserve of eggs or their excess.
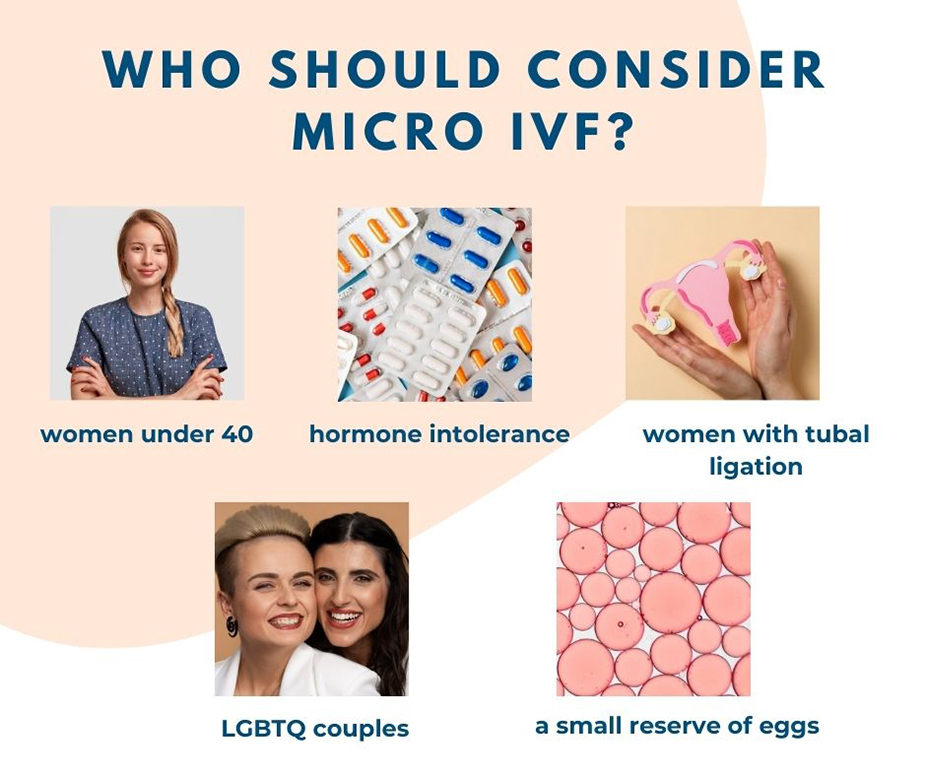
If you are considering mini IVF for conception, consult with a fertility specialist to make sure this protocol will work for you.
Mini IVF Success Rates Under and Over 40
The success in conception depends on many factors. The quality of your eggs and sperm, the medical condition of your uterus and cervix, hormones, and dietary habits affect pregnancy.
Although younger patients show better results, women over 40 also have a chance to have a baby. Check out the statistics of mini IVF success rates over 40 and under this age. It is based on the CLBR, Cumulative Live Birth Rate, after the first and third cycles, and the LBR, Live Birth Rate, per oocyte for all age groups.
| Age Group | Mean Oocytes Retrieved | CLBR (First Cycle) | CLBR (Third Cycle) | LBR per Oocyte |
|---|---|---|---|---|
| ≤ 34 years | 1.5 | 42.5% | 70.1% | 9.6% |
| 35–37 years | 1.5 | 32.9% | 49.1% | 9.6% |
| 38–40 years | 1.5 | 20.0% | 38.6% | 9.6% |
| 41–42 years | 1.5 | 12.6% | 25.2% | 9.6% |
| ≥ 43 years | 1.5 | 4.4% | 8.8% | 9.6% |
Mini IVF Success Stories
Do not rush to get upset if you are in your 40s and cannot get pregnant with low stimulation. The story of the conception of Lisa and Lynsey proves that everything is possible! This lesbian couple chose gentle IVF, thanks to which the woman was able to get pregnant at the age of 39.
In this cycle, I took only folic acid and vitamin D. My estrogen increased progressively, and it was enough to transfer the embryo and prepare my reproductive system for carrying a child. I am very happy!
Today, the family has two children and is happy to share their experience.
Mini IVF Cost
The microprogram is usually more affordable. The difference in cost is achieved due to a reduced protocol of medications.
However, there are also disadvantages. In the long term, this method may not be as cost-effective. Getting fewer high-quality eggs reduces the number of embryos that freeze for future cycles. Very often, there are no leftovers at all. Then, if a woman wants to get pregnant with a second child, she will have to go through the entire program all over again, which significantly increases the cost.
If you have chosen a gentle protocol, here are the approximate sums the treatment will cost you.
| Item | Estimated Cost (USD) |
|---|---|
| Medications | $500 - $2000 |
| Monitoring (ultrasounds, blood tests) | $1000 - $1500 |
| Procedure | $3500 - $4500 |
| Total Estimated Cost | $5000 - $8000 |
Mini IVF FAQ
Mild IVF is based on gentle treatment and involves the use of preoral medications. That is why you can get by with only 1-2 injections during the entire program.
Yes. It is efficient after tubal ligation, as the program does not involve interaction with fallopian tubes. Instead of passing the embryo through the fallopian tubes, the doctor transfers it to the uterus. Thus, a woman with the pathology has every chance of getting pregnant.
Mild stimulation allows you to get 3-6 high-quality oocytes. However, there is no evidence that these gametes will be better than with the standard treatment.
Summary
To sum up, we consider mini IVF a good idea for those who want to avoid many injections and prevent the negative effects of hormonal drugs. It reduces the cost of medications and minimizes harm to the body. However, you should consider that this method may be irrelevant for some patients. In some cases, it can’t lead to a conception.
If you are looking for the most optimal IVF program and want to know if gentle stimulation is for you, contact our specialists for detailed advice on these and other issues.