Diminished Ovarian Reserve – Causes, Diagnostics, Treatment
A low/diminished ovarian reserve means that a woman’s ovaries have few eggs that can reach maturity and fertilize. Each woman is born with a certain individual number of oocytes; this is the ovarian reserve. With each ovulation, there is a gradual reduction of this reserve. Still, in addition to the physiological one, there is also a pathological decrease in the ovarian reserve, which further leads to problems with the onset of pregnancy and a decrease in fertility.

Today we will learn the reasons that cause diminished ovarian reserve, its diagnostics, treatment, and pregnancy chances. Let`s start with a general overview and definition of this condition.
What Is Diminished Ovarian Reserve (DOR)
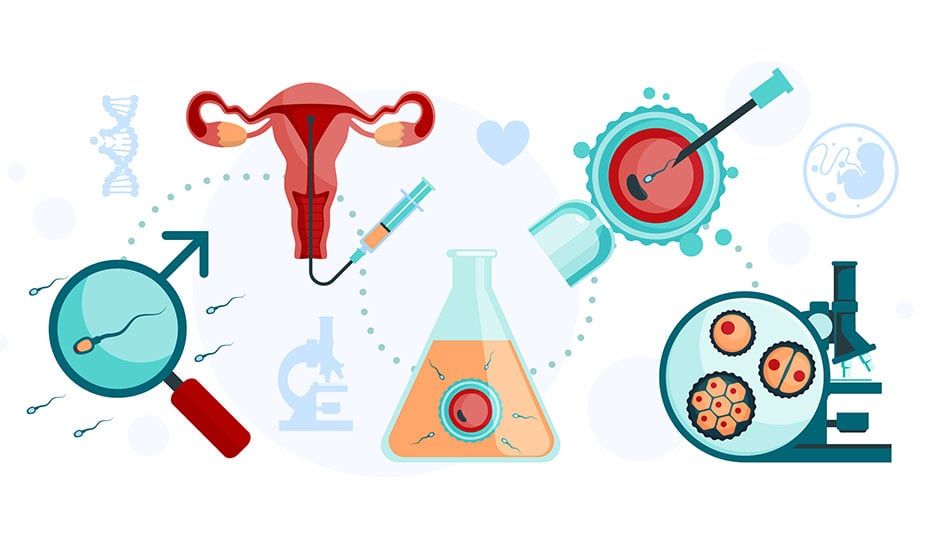
Ovarian reserve or follicular reserve is the number of eggs that can participate in the fertilization process. Low ovarian reserve is one of the most common causes of infertility and IVF failure.
The ovarian reserve is assessed by a fertility specialist based on the results of ultrasound and laboratory tests. A diminished / low ovarian reserve means that a woman’s ovaries have few eggs that can reach maturity and fertilize.
- Ovarian reserve begins to decline at age 30 or even earlier and declines rapidly after age 40.
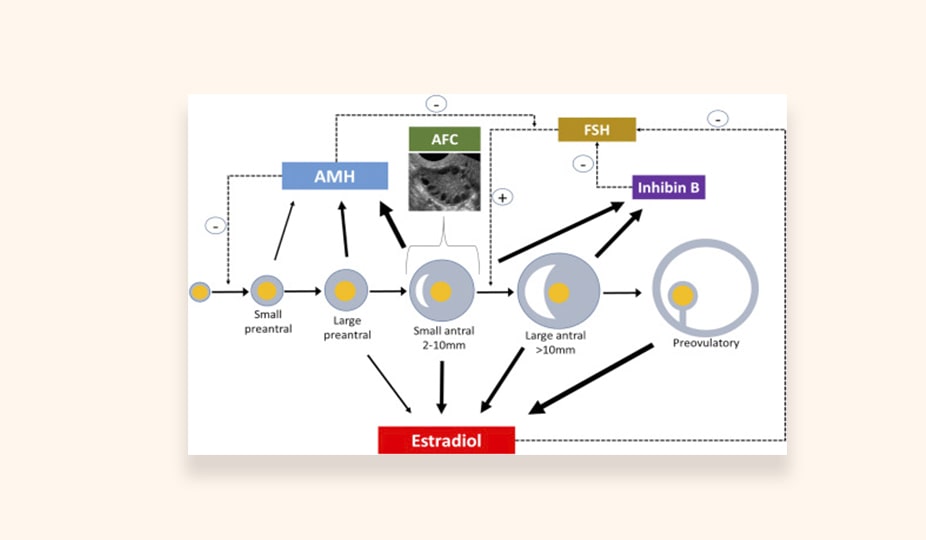
- Testing for reduced ovarian reserve should begin by measuring FSH or estradiol levels, but anti-Müllerian hormone (AMH) and antral follicle count (AFC) should be measured to confirm the diagnosis.
- If the woman is more than 42 years old or ovarian reserve is reduced, she should consider assisted reproductive technologies with donor oocytes.
The development of assisted reproductive technologies has led to the fact that the ovarian reserve and its decrease are considered from the standpoint of the ovarian response to the effect of gonadotropic drugs. Gonadotropins are a group of drugs that affect the reproductive glands, including those that promote follicles’ maturation in the ovaries. Normal ovarian reserve is an adequate response of the ovaries to stimulation. An adequate response refers to the required follicular growth and the production of a sufficient number of oocytes. A sufficient number is determined by the general number of oocytes and the number of embryos obtained after fertilization with the correct chromosome set.
Symptoms of a Decreased Ovarian Reserve
Decreased ovarian reserve is a prolonged process that most often occurs without symptoms. The reason that makes a woman see a doctor is the absence of pregnancy (infertility).
The most striking symptoms that characterize diminished ovarian reserve are estrogen deficiency signs, such as hot flashes, sweating, tachycardia, and, over time, amenorrhea before the age of 40.
Diminished Ovarian Reserve Causes
The reasons for the decrease in the number and quality of eggs are as follows.
Age
Age is a key physiological factor that determines the gradual decline in ovarian reserve. With an increase in reproductive age, the number and quality of oocytes decrease. Besides, unlike other cells in the body, germ cells do not regenerate. 95% of women at the age of 30 have only 12% of oocytes from their initial number, and by 40 years – only 3%. Infertility problems are most effectively solved before the age of 34 and not always with the help of IVF.
Postponed diseases and operations
For example, removal of cysts, uterine fibroids, endometriosis treatment. Any surgical intervention on the ovaries leads to a significant decrease in the ovarian reserve and, consequently, decreased effectiveness of assisted reproduction methods. Until recently, one of the most frequent interventions in the treatment of polycystic ovary syndrome was surgery excision of at least 2/3 of the ovarian tissue. An even more traumatic and unjustified surgical tactic is the surgical treatment of retention cysts of the ovaries.
The consequence of such operational tactics is the loss of a significant part of the ovary’s functional tissue. Today, such interventions are quite rare. Interventions (appendectomy, removal of retention cysts of the ovaries, restoration of patency of the fallopian tubes, coagulation of endometriosis foci) often lead to an adhesive appearance process in the small pelvis. The adhesion process causes vascular changes, a violation of ovarian tropism, and negatively affects the ovarian reserve.
Intoxication
The intoxication of the body due to excessive smoking, drinking alcohol, drugs. Tobacco smoking has a significant negative role on the ovarian reserve. It has been shown that the toxic effect of nicotine on the ovaries is manifested in the acceleration of the processes of apoptosis (death) of follicles, which is manifested by a decrease in the concentration of the level of AMH (anti-Müllerian hormone). Drinking alcohol has a similar effect.
Impact of chemicals used in industry and agriculture
As a historical reference, the toxic effects on the reproductive function of dichlorodiphenyltrichloroethane and diethylstilbestrol, which are analogous to estrogens in their chemical structure, should be mentioned. These components affect the female fetus even in utero.
Mumps
There is an assumption that girls who had recovered from mumps, in parallel, asymptomatically suffered inflammation of the ovaries, which contributed to the accelerated death of follicles.
Heredity (genetic reasons) and endocrine system malfunctions
- aneuploidy (presence of an additional or absence of one chromosome) and structural rearrangements of the X chromosome;
- Turner syndrome and other diseases associated with disorders of the embryonic development of the gonads;
- fragile X syndrome (FXS) – a mutation in the FMR1 gene on the X chromosome;
- the presence of autosomal genetic mutations (galactosemia);
- autoimmune diseases – the presence of antibodies to cells that synthesize sex hormones (Addison’s disease) and autoimmune diseases of the thyroid gland.
Low Ovarian Reserve Diagnostics
Diagnostics is based on a combination of anamnestic and clinical and laboratory data. The most important thing is age. Clinical manifestations of a decrease in ovarian reserve often begin to appear after 35 years.
Very often in the anamnesis, there is a mention of the early onset of menopause in the closest female relatives (mother, older sisters).
Ultrasound
With its help, specialists can estimate the ovaries’ volume and calculate the number of antral follicles (resting follicles). Their size is up to 8 mm, and the number coincides with the number of primordial (primary) follicles, which are the precursors of eggs. AFC (antral follicle count) is the total number of follicles counted over an area of 2 to 10 mm (mean diameter) in both ovaries during the early follicular phase. Doctors determine AFC via observation during the transvaginal ultrasound. If the AFC is low (from 3 to 10), pregnancy after IVF is less likely.
If the number of antral follicles is less than normal, ovarian response to stimulation is weak. In this case, the onset of natural pregnancy is unlikely, and there is a need for IVF.
Laboratory Test
The ovarian reserve is assessed by a fertility specialist based on the results of ultrasound and laboratory tests. Laboratory tests determine the level of blood hormones.
- Follicle-stimulating hormone (FSH) and luteinizing hormone (LH). Laboratory test detects them in the first phase of the menstrual cycle (2-3 days). There is a direct relationship between the level of these hormones and follicular storage. An increased FSH is the first sign of a decrease in ovarian reserve. FSH levels > 10 units/ml or estradiol levels <80 pg/ml on day 3 of the menstrual cycle suggest a decrease in ovarian reserve.
- AMG (anti-müllerian hormone). Low levels of AMH in the blood coinsides with a small number of follicles in the ovaries. AMH levels do not change with the menstrual cycle. Hormone level is an early, reliable predictor of decreased ovarian function. Consequently, low AMH levels indicate a reduced chance of pregnancy after in vitro fertilization (IVF). Pregnancy with women`s own oocytes is almost impossible if the level is too low.
- INHBB (Inhibin B). Determination of this hormone’s level makes it possible to predict the ovaries’ response to the stimulation of superovulation and, consequently, the success of IVF. A decrease in inhibin A and B levels signals the reproductive system aging.
Low Ovarian Reserve and Woman`s Age
Low ovarian reserve is usually found in women of late reproductive age – after 35 years.
At the birth of a girl, the number of follicles in her ovaries reaches two million. By the beginning of puberty, there are 200-400 thousand of them.
After the age of 30, a woman’s ovarian reserve begins to decrease.
After 35 years, the number of eggs decreases rapidly, and it becomes more difficult to get pregnant both naturally and with assisted reproductive technologies.
Is It Possible to Get Pregnant with Diminished Ovarian Reserve
Women with a low follicular reserve have a poor response to the superovulation stimulation carried out at the first IVF stage. In this case, it is not always possible to retrieve oocytes (empty follicle syndrome).
However, even if there are enough oocytes, they are not ready for fertilization due to poor quality. Fertilization with low egg quality is possible, but the embryo will most likely not be viable. They can have genetic abnormalities and either stop their development or lead to pregnancy with complications or a miscarriage.
Therefore, with a low ovarian reserve, sometimes it is necessary to use donor eggs.
It is possible to preserve your own young egg until pregnancy at a late reproductive age using cryopreservation.
Diminished Ovarian Reserve Treatment and Prophylaxis
There is no pathogenetic cure. Therapy aims primarily to eliminate the consequences of a decrease in the ovarian reserve, namely, overcoming infertility.
DOR Treatment
In assisted reproduction programs, depending on the patient’s belonging to a particular group, experts use various stimulating therapy strategies to obtain more oocytes.
As a result of the introduction of these categories, they distinguish four groups of patients with a reduced ovarian reserve and a low response to stimulatory therapy.
First group:
- age up to 35 years;
- the number of antral follicles (CAF) is more than 5;
- AMH is greater than or equal to 1.2 ng/ml.
Second group:
- over 35 years old;
- CAF more than 5;
- AMH is greater than or equal to 1.2 ng/ml;
- unexpectedly poor response to standard IVF stimulation.
Third group:
- age up to 35 years;
- CAF less than 5;
- AMH less than 1.2 ng/ml.
Fourth group:
- over 35 years old;
- CAF less than 5;
- AMH less than 1.2 ng/ml.
For the first and second groups, five main strategies are used, separately or in combinations:
- priority in the use of recombinant FSH (follicle-stimulating hormone) in comparison with gonadotropins obtained from the urine;
- increasing the single and total dose of FSH for stimulation;
- the use of recombinant LH (luteinizing hormone);
- adding the steroid hormone dehydroepiandrosterone (DHEA) before ovarian stimulation;
- application of the double stimulation protocol (DuoStim).
The most difficult for obtaining a sufficient number of oocytes are patients belonging to the third and fourth groups.
The strategies proposed for stimulating patients of the third and fourth groups:
- application of individual stimulation protocols – minimal, low-dose stimulation, natural cycle (obtaining eggs without ovarian stimulation);
- an individual strategy for an ovulation trigger (it can be, for example, human chorionic gonadotropin or a gonadotropin-releasing hormone agonist);
- the use of adjuvant (additional) preliminary therapy.
Despite the active use of low-dose protocols, recent studies support the idea of high-dose stimulation of recombinant FSH with the addition of recombinant LH.
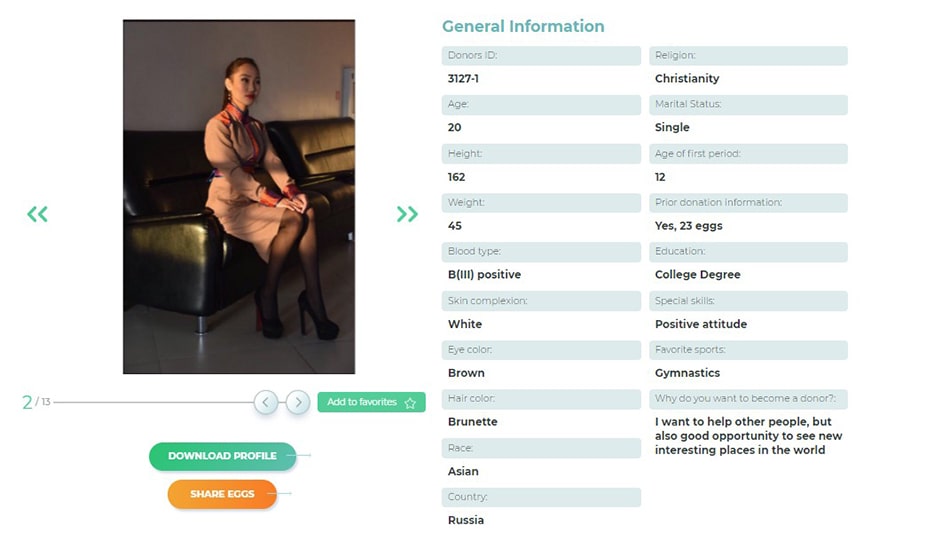
If it is impossible to obtain a sufficient number of oocytes, the use of donor oocytes is recommended. There is an international egg donors database, you can create a free account and find a perfect donor yourself, or contact us to get free consultancy of the best fertility experts.
DOR Prophylaxis
With a critical decrease in ovarian reserve and the onset of climacteric changes, it is necessary to use hormone replacement therapy. Doctors carry it out to prevent the musculoskeletal system’s complications (osteoporosis), disturbances in the body’s electrolyte balance, and the development of diseases of the cardiovascular system.
For the prevention of infertility, specialists recommend to do the following.
- Plan and implement reproductive function up to 35 years old, especially for women at risk (early maternal menopause, endometriosis, ovarian surgery);
- Eliminate bad habits (smoking, drinking alcohol);
- Oocyte or embryo banking is a woman doesn`t plan pregnancy and childbirth until 35 years, or before the upcoming chemotherapy and/or radiation therapy in case of cancer treatment.
Prevention of iatrogenic complications is as follows.
- Reduce surgical interventions where it is possible to apply conservative therapy;
- If ovarian surgery is necessary, take care of the ovarian tissue as carefully as possible.
Summing Up
Treatment and tactics of achieving pregnancy are individual and depend on the woman’s body, age, and hormonal status. Women with low ovarian reserve often require IVF programs with their own or donor oocytes. You can get the best advice concerning your ovarian reserve and start planning a pregnancy with our experts. Sunshine team is always here to help, and we will gladly answer all your questions via email, WhatsApp, WeChat, or phone call.