How Many Eggs Are Normal during Egg Retrieval – IVF Statistics
Oocytes are precious gems from the IVF perspective. Now, most reproductologists share the opinion that a perfect number of eggs during IVF retrieval is 15. However, this amount strongly depends on the woman`s age. More than that, in most cases, it is better to receive 1-2 healthy oocytes than a dozen of low-quality cells. In this post, we will explain how the IVF success with own and donor eggs depends on their quality, quantity, and the woman`s age.

What is IVF and How It Helps to Resolve Fertility Issues
Now, to conceive a child, more and more married couples require the latest medical technologies. Almost 20% of people of reproductive age (15–49 y.o. for women, over 16 y.o. for men) cannot get pregnant without the help of reproductive specialists. How can doctors help?
IVF, or in vitro fertilization, is a reproductive technology in which the processes of egg fertilization and the initial stages of embryo development occur in laboratory conditions, that is, in a test tube. The IVF cycle (or protocol) includes stimulation of the ovaries to produce the maximum number of eggs, puncture (collection of oocytes, eggs), fertilization of an egg with sperm in a test tube, and embryo transfer into the uterine cavity.
About a million transfers are made in China every year, 600,000 in Europe, 500,000 in Japan, and 200,000 in the United States. The expert community expects an increase of 5-7% per year.
In scientific circles, there is no alternative to IVF.
IVF Protocole Explained
On average, 25–33% of IFVs are successful. Specialists say that the younger the patient, the higher the likelihood of IVF conception – up to 40%.
That is, under the most favorable circumstances, each couple goes through several protocols, IVF rounds, before getting pregnant.
The IVF protocol begins with an examination of the prospective parents. Statistics show that in 50% of cases, pregnancy does not occur due to the female factor. Another 50% happens due to the male fertility factor. At the same time, in 30-40% of cases, in couples with a predominantly female or male infertility factor, both parents have certain problems that interfere with the onset of pregnancy.
The IVF cycles, or protocols, follow the same pattern. Doctors accelerate a woman, like an airplane on a runway, with hormone therapy to obtain a healthy dominant follicle. A follicle is a small sac of fluid in which one egg locates and matures, surrounded by helper cells, i.e., follicular cells. They are oocytes. A woman grows one dominant follicle in the natural period; however, she can develop five, ten, or even twenty oocytes during one stimulated cycle with hormonal therapy. For successful fertilization, one needs as many follicles as possible.
During the maturation of oocytes, doctors regularly examine the woman. If there is no growth, the protocol is interrupted. With normal development, doctors schedule the retrieval day. During this day, they inject the medication that causes ovulation. The fertility specialist pierces the follicle and draws out the fluid. The embryologist receives those tubes and looks for the egg under a microscope. The eggs are fertilized with sperm and placed in an incubator, where they either freeze or continue to divide actively.
On the fifth day, doctors transfer one or more embryos into the uterine cavity. Excess embryos are frozen and sent for storage to a cryobank.
How Many Eggs Does a Woman Need for Successful Pregnancy by Age
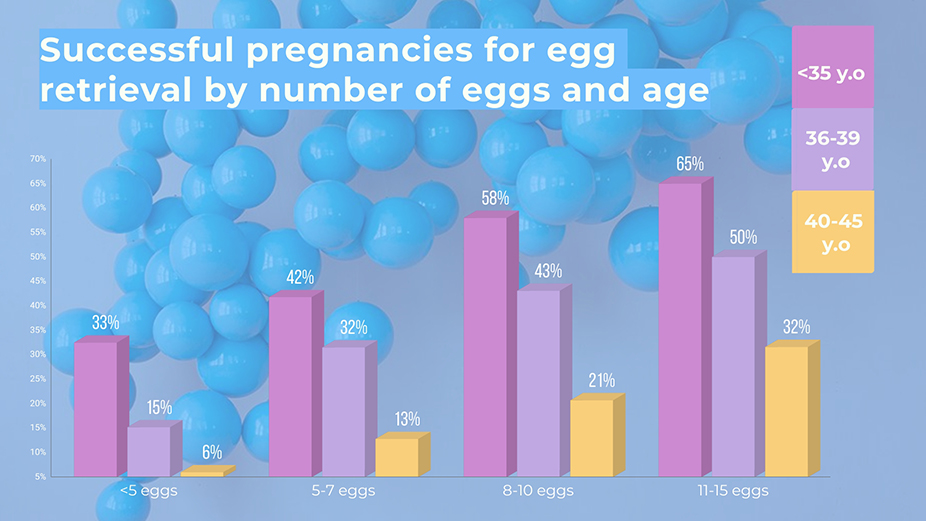
According to statistics:
- women under 35 years old need nine oocytes to get one embryo;
- 35–37 years old – about 12 oocytes;
- under 42 years old – 16;
- over 42 years old – an average of 100 oocytes.
Ovarian Reserve and Fertility
A follicle is an egg surrounded by epithelial cells. Women have a limited number of follicles at birth. Each girl is born with a reserve of 400,000 – 500,000 oocytes, follicles. However, most of them leave unused. On average, a woman ovulates around 400 times during her life. A woman’s reproductive life lasts approximately 40 years. A woman can go off follicles at 35 years old or at 55; the low ovarian reserve is individual.
The average statistical age of menopause is 51 years and six months. Still, sometimes follicular supply begins to decrease from 27 years old. When the process starts, it is impossible to force the woman’s body to produce more follicles. Reproductive experts are joking that loving parents should give their daughter at the age of majority not a 10-carat diamond, but a certificate for eggs cryopreservation.
How to Evaluate the Embryo Quality – Does the Number of Eggs Really Matter?
Like diamonds in the hands of a cutter, all embryos are graded on an alphanumeric scale. For example, the Gardner scale consists of a number and two letters. The number characterizes the volume, letters from A to D – the inner and outer cell mass. Like a diamond, an AA-grade embryo is considered excellent.
Since during IVF, doctors usually get several embryos, they can select the most viable ones.
On average, up to the fifth day of cultivation, 50-60% of fertilized oocytes survive. Some embryologists are confident that the third day is perfect for embryo transfer and adaptation. But one cannot ignore the fact that some of the embryos can stop in development on the third, fourth, and fifth day. Laboratories with extensive cultivation practice tend to postpone the process of embryo transfer.
In addition, it is on the fifth or sixth day that they can perform an embryo biopsy, i.e., PGS preimplantation genetic screening.
According to statistics in women under 35, the proportion of embryos capable of producing healthy children is 59%, 35-40 years – 41%, and in the group over 40 years old – 20%. The main goal of PGS is to increase the likelihood that a healthy pregnancy will occur and will continue.
World statistics state that the frequency of pregnancy after testing an embryo with PGS increases by at least one-third.
How to Choose the Best Donor to Receive a Sufficient Number of Eggs
Many clinics and cryobanks are trying to expand the donor’s profile. In addition to standard criteria, we additionally request a voice sample, children’s photographs, and create a psychological portrait. We carry out genetic diagnostics – this helps clients choose their biological mother in a meaningful way, reducing the number of risks.
In the competition of cryobanks, the winners provide the widest selection of biomaterials by blood group, phenotype, nationality, and even zodiac signs.
The requirements for donors are severe, with only one out of three hundred candidates left. First, we exclude carriers of dangerous mutations. The biological activity of the material is very important. It is necessary to undergo a cryotest when the egg is frozen and thawed. Finally, the psychologist excludes candidates with mental disabilities.
Number of Embryos that Is Good for Pregnancy
Initially, IVF technology involved multiple pregnancies. Having selected the most active embryos, the reproductive specialist transferred them into the uterine cavity. Typically, there are three to four embryos, sometimes six. This was done as a safety net so that at least one would lead to pregnancy. In the case of multiple pregnancies, several embryos will have to be reduced.
The issue of the ethics of this action has not yet been resolved. In America, in 2009, Nadya Suleman gave birth to 8 children, having previously signed an agreement with a reproductologist for an experiment, according to which the doctor relinquished responsibility for the life and health of the mother and children. In 2008, five girls were born to the Moscow Orthodox Artamkin family. The birth took place in London.

Now the transfer rates are one or two embryos. We limit the number of embryos transferred to two. Unfortunately, with the transfer of one embryo, the frequency of successful pregnancies decreases. Of course, in some cases, we also transfer three fertilized eggs. E.g., when a woman is 44 years old and the probability of pregnancy is low, we, with her consent, transfer three embryos. Yes, triplets may occur, and reduction may be necessary.
Modern IVF technologies allow people to achieve good results when transferring one embryo. Our task is to explain to the patient why it is unnecessary to use more than two embryos (in some cases, more than one). Another thing is that embryos often divide, and we still lead to multiple pregnancies. For young women who don`t have serious illnesses, we are now generally trying to transfer one embryo at a time.
Fertility Tourism
Residents of the EU, the USA, and Australia are actively interested in the conditions and cost of IVF in Russia, Cambodia, and Malaysia.
In the USA, the transfer rate in patients over 40 y.o. is 2%. In Russia – about 12%. However, Europeans and Americans do not go to Russia for IVF, despite the obvious cheapness (for comparison: an IVF cycle in a Moscow clinic costs about $3000 without hysteroscopy and PGS, and in the USA, one protocol costs about $10000 + $5000 for stimulation drugs.
Patients from Europe and China, where there are significant restrictions on these procedures, mainly apply for donor material, surrogacy programs, and preimplantation genetic diagnostics. If you have any questions regarding the IVF procedure, the quantity, and the quality of oocytes required for a successful program, write to us, and we will provide you with a free consultation.